Availity Clearinghouse Rejection Codes - To determine whether any of the payers that you submit to require a contract, see the availity payer list. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
8 Common Clearinghouse Rejection Codes Debunked — Etactics
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Clearinghouse Rejection Codes Explained [Latest 2025]
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Meet Availity Our New & Improved Clearinghouse 30 less than current
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Check Rejections in Availity
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Clearinghouse Rejection Codes & How To Fix Them? BMB
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare.
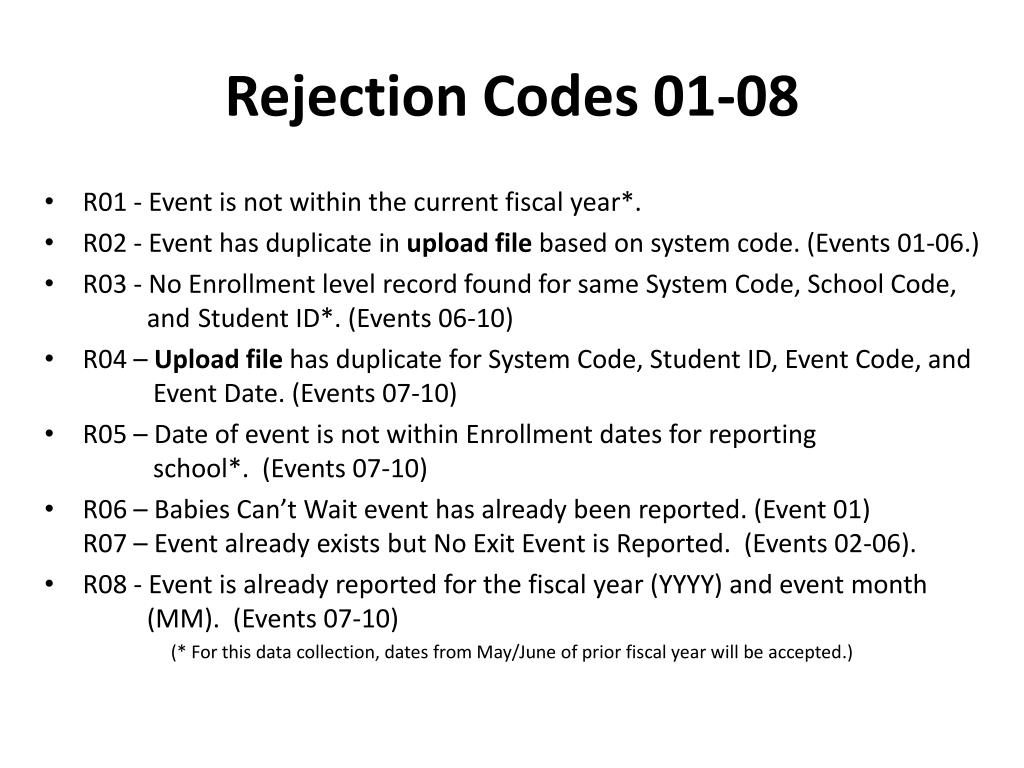
PPT Cultivating the Special Education Event Garden PowerPoint
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
8 Common Clearinghouse Rejection Codes Debunked — Etactics
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Availity Simplifies Payer Connectivity And Claim Submission With Expert Support For Edi Transactions, Payer Ids, And Healthcare.
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.

![Clearinghouse Rejection Codes Explained [Latest 2025]](https://rcmfinder.com/wp-content/uploads/2025/01/Clearinghouse-Rejection-Codes-Explained.jpg)


![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/02/what-is-an-entity-code-rejection.jpg)
![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/10/blog-Fi.jpg)

![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/10/blog-info-1-905x1024.jpg)